Ototoxic denotes toxic to the ears (oto-). Ototoxic drugs are concentrated in the labyrinthine fluid. When the plasma concentration falls, these are gradually eliminated from the labyrinthine fluid. Ototoxicity is worse when the drug’s plasma concentration is consistently high and above a threshold value. Reduced renal clearance can predispose ototoxicity of the drug. The most ototoxic potential is shown in aminoglycosides.
The inner ear serves two functions, auditory (hearing) and vestibular (postural balancing of the body).
Cochlear (auditory) damage: Hearing loss affects high frequency sound initially, then gradually involves lower frequencies; it begins at the base and spreads to the apex of cochlea. Patients who are older and who already have a hearing loss are more vulnerable. The cochlear toxicity is first asymptomatic and can only be identified through audiometry. Tinnitus then appears, followed by progressive hearing loss. On stopping the drug, tinnitus disappears in 4–10 days, but frequency loss persists.
Vestibular (postural balance) damage: Headache is usually first to appear, followed by nausea, vomiting, dizziness, nystagmus, vertigo and ataxia. After discontinuing the drug, recovery (often incomplete) may take 1-2 years. The age of the patient and the severity of the initial injury determine how permanent the alterations will be (elderly have poor recovery).
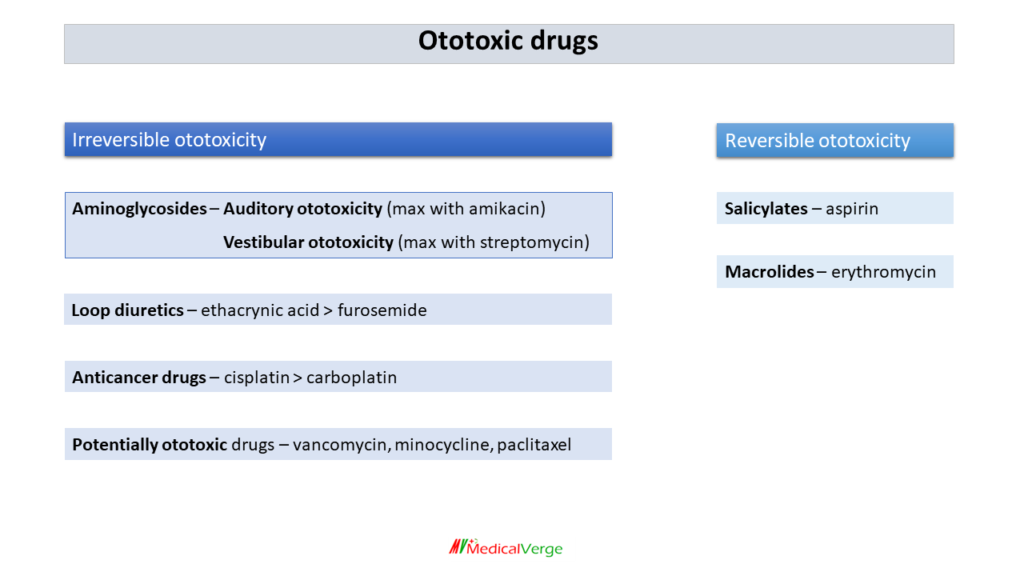
Irreversible ototoxicity
Aminoglycosides – Auditory ototoxicity (max with amikacin)
– Vestibular ototoxicity (max with streptomycin)
Loop diuretics – ethacrynic acid > furosemide
Anticancer drugs – cisplatin > carboplatin
Potentially ototoxic drugs are vancomycin, minocycline and paclitaxel, chloroquine/hydroxychloroquine, although there is little clinical proof of potentiated ototoxicity. Concurrent use of these drugs may increase the risk of ototoxicity (ototoxic synergism).
Reversible ototoxicity
After discontinuing drugs for a few days or weeks, ototoxicity returns to normal.
salicylates – aspirin
macrolides – erythromycin