Antiemetics are drugs used to prevent vomiting. Vomiting is a protective mechanism of GIT/stomach to expel out undesired or hazardous foods or chemicals. It is an innate protective reflex rather than a disease, while nausea is the sense of vomiting. Sometime undesirable vomiting can occur due to emotional stress, motion sickness, therapeutic drugs like anticancer, diseases like gastroenteritis, where vomiting has to be suppressed. Numerous therapeutic targets are discovered and suggested for antiemetic agents by understanding the mechanism of emesis.
Mechanism of emesis (vomiting)
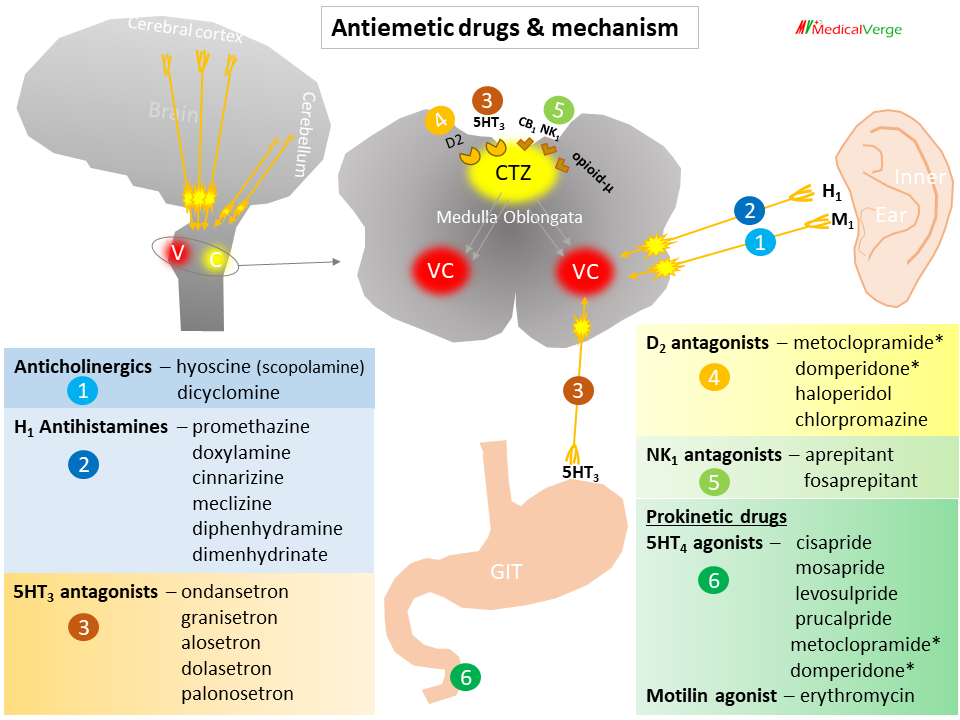
Vomiting occurs due to stimulation of the emetic (vomiting) centre situated in the medulla oblongata. Multiple pathways can elicit vomiting –
Chemoreceptor Trigger Zone (CTZ) is the most important relay areas for afferent impulses arising in the g.i.t, throat and other viscera. Because the CTZ is not shielded by the blood-brain barrier, it is potentially susceptible to drugs, mediators, hormones, toxins, etc. that are carried in the blood. The CTZ and NTS exhibit a number of emesis signaling receptors, including histamine H1, dopamine D2, serotonin 5-HT3, cholinergic M1, neurokinin NK1 (activated by substance P), cannabinoid CB1, and opioid μ receptors that may be the targets of antiemetic drug action.
Cytotoxic drugs, radiation, and other gastrointestinal irritants cause the release of serotonin (5HT) from enterochromaffin cells. The enteric nervous system’s extrinsic primary afferent neurons have 5-HT3 receptors, which are where the 5HT binds. These neurons connect with vagal and spinal visceral afferents to send impulses to CTZ. Large amounts of 5-HT released could also leak into the bloodstream and circulate via the blood vessels to reach CTZ.
Inflammatory mediators may also cause platelets to produce 5-HT. While substance P and other messengers are also involved, 5-HT is not the only peptide that mediates these signals.
The vestibular apparatus generates impulses when body is rotated or equilibrium is disturbed or when ototoxic drugs act. These impulses reach the vomiting centre mainly relayed from the cerebellum and utilize muscarinic as well as H1 receptors.
Numerous unpleasant sensory stimuli, including strong odors, frightening sights, excruciating pain, anxiety, memories of annoying events, and anticipation of an emetic stimulus (repeated dosage of cisplatin), trigger nausea and vomiting through the higher centre.
Antiemetic drugs classification
- Anticholinergics – hyoscine (scopolamine), dicyclomine
- H1 Antihistamines – promethazine, doxylamine, cinnarizine, meclizine, diphenhydramine, dimenhydrinate
- 5HT3 receptor antagonists – ondansetron, granisetron, alosetron, dolasetron, palonosetron
- D2 receptor antagonists – metoclopramide*, domperidone*, Neuroleptics (haloperidol, chlorpromazine, prochlorperazine)
- NK1 receptor antagonists – aprepitant, fosaprepitant
- Prokinetic drugs (hurrying gastric emptying)
5HT4 receptor agonists – cisapride, mosapride, levosulpride, prucalpride, metoclopramide*, domperidone*
Motilin receptor agonist – erythromycin
Uses (etiology-based drug selection)
Motion sickness
The vestibular system is an inner ear organ that detects motion (acceleration) in all three dimensions of the body and sends signals to the cerebellum to keep the body balanced. Specifically, cholinergic (M1) and histaminergic (H1) neurons are involved in this neural circuit. In some people overactivity of these pathway during travelling manifested as vomiting called motion sickness. The first choice for treating motion sickness is an anticholinergic and an antihistaminic. All anti-motion sickness drugs act better when taken ½–1 hour before commencing journey. Hyoscine (0.2–0.4 mg oral or IM) is the most effective drug for motion sickness. A transdermal patch delivering 1.5 mg of hyoscine over the course of three days has been designed. When applied behind the pinna, it prevents motion sickness while exhibiting only mild side effects. Dicyclomine (10–20 mg oral) has been recommended for the prophylaxis of motion sickness and morning sickness.
Morning sickness (vomiting of early pregnancy/hyperemesis gravidarum)
Antihistaminics may be teratogenic, however there is no concrete evidence to support this. The majority of morning sickness instances can be treated with reassurance and dietary modifications. Low dosages of dicyclomine, promethazine, prochlorperazine, or metoclopramide may be administered if an antiemetic is necessary. Doxylamine is an H1 antihistaminic sedative with strong anticholinergic action. Although it is not used for morning sickness in the UK or many other countries, it is explicitly advertised in India in combination with vitamin B6. 10-20 mg at bedtime, with additional doses may be given in morning and afternoon if necessary. Oral absorption of doxylamine is slow, has a half-life of 10 hours.
Drug (cancer chemotherapy/radiotherapy) induced vomiting
Cytotoxic drugs or radiation induce nausea and vomiting by causing cellular damage, which causes release of mediators including 5-HT and substance-P from intestinal mucosa. 5-HT activate vagal afferents in the gut to send emetogenic signal to CTZ/NTS as well as spill into circulation and reach CTZ via the vascular route. 5HT3 antagonists like ondansetron blocks emetogenic impulses both at their peripheral origin and central relay. Hence 5HT3 antagonists are 1st choice for drug induced vomiting. Cisplatin is the most emetogenic drug ever. NK1 receptor antagonist that blocks the emetic action of substance P, can be used as adjuvant antiemetics.
Post-operative nausea and vomiting (PONV)
Ondansetron and other 5HT3 antagonists are still the first choice because they were found to be very effective in PONV. NK1 receptor antagonists may be used alone or in combination with other treatments. It is asserted that a single (40 mg) oral dose of aprepitant is equally effective as ondansetron for PONV.
Disease induced vomiting (gastroenteritis, liver disease)
5HT3 receptor antagonists are 1st choice. Neuroleptics (phenothiazines, haloperidol) can be used, have broad spectrum antiemetic action. Neuroleptics antagonize apomorphine induced vomiting and have additional antimuscarinic as well as H1 antihistaminic property. Prokinetic drugs like metoclopramide, domperidone, mosapride have prominent 5HT4 agonist property, can exacerbate diarrhea in gastroenteritis.
Contrast between 5HT3 and 5HT4 receptor
5HT3 and 5HT4 both are serotonin (5HT/ 5-Hydroxytryptamine) receptor subtypes, each have distinct functions. There are 5 clinically important subtypes of serotonin receptors (5HT1A, 5HT1B, 5HT2A/2C, 5HT3 and 5HT4) that are implicated in various systems or disorders. Only 2 receptor subtypes, which are briefly discussed below, are involved in GIT.
5HT3 receptor is involved in emesis, blocking of which result in suppression of vomiting. while 5HT4 is involved in gastrointestinal movement (peristalsis), stimulation of which causes gastric emptying. 5HT3 antagonist show their antiemetic action directly by blocking serotonergic neuron pathway involved in emesis (vomiting), while 5HT4 show their antiemetic action indirectly by the virtue of promoting forward movement of food contents (gastric emptying) called prokinetic action.