H1 antihistamines compete with histamine to block its effects at H1 receptors, such as cetirizine, promethazine, pheniramine, azelastine etc. They have antiallergic actions while have poor antipruritic, antiemetic and antitussive actions. According to recent research, the H1 receptor has some constitutive activity, and H1 antihistaminics also possesses inverse agonistic action.
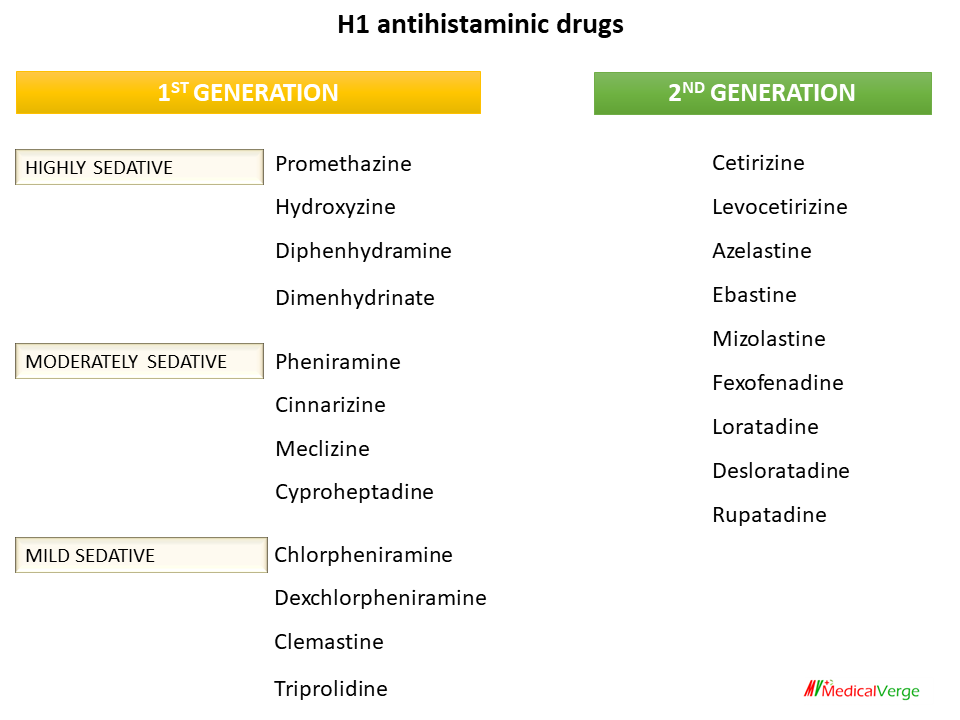
H1 ANTIHISTAMINES CLASSIFICATION
1st generation H1 antihistaminics
HIGHLY SEDATIVE – Promethazine, Hydroxyzine, Diphenhydramine, Dimenhydrinate
MODERATELY SEDATIVE – Pheniramine, Cinnarizine, Meclizine, Cyproheptadine
MILD SEDATIVE – Chlorpheniramine, Dexchlorpheniramine, Clemastine, Triprolidine
2nd generation H1 antihistaminics
Cetirizine, Levocetirizine, Azelastine, Ebastine, Mizolastine, Fexofenadine, Loratadine, Desloratadine, Rupatadine
PHARMACOLOGICAL ACTIONS
Action on smooth muscle
H1 antagonists block the majority of histamine’s actions on smooth muscles, particularly constriction of respiratory smooth muscle. They significantly prevent histamine-induced bronchoconstriction, intestinal and other smooth muscle contractions.
At presence of lower dosages of histamine, H1 antagonists block the immediate vasodilator effects mediated by activation of H1 receptors on endothelial cells (synthesis/release of NO and other mediators). They help to prevent venous constriction, which can occur in some vascular beds. Low-dose histamine-induced falls in blood pressure are prevented, while additional H2 antagonists are required for complete blockade of that caused by higher doses. Adrenaline release from the adrenal medulla in response to histamine is blocked. Histamine-induced constriction of bigger blood vessels is also inhibited. These drugs have no effect on the action of histamine on gastric secretion.
Action on capillary permeability
H1 antagonists effectively prevent histamine-induced enhanced capillary permeability and the genesis of oedema and wheal.
Antiallergic action
Most manifestations of immediate hypersensitivity (type I reactions) are suppressed. Itching urticaria and angioedema are well controlled. Anaphylactic fall in BP is only partially prevented. The antihistaminics are ineffective in bronchial asthma because Leukotrienes (C4, D4) and PAF are more important mediators than histamine and concentration of antihistamines attained at the site may not be sufficient to block high concentration of histamine liberated locally in the bronchi. However Certain newer agents like cetirizine have adjuvant role in seasonal asthma.
Action on CNS
Antihistamines cause different levels of CNS depression. This appears to be dependent on the compound’s potential to cross the blood-brain barrier as well as its affinity for central H1 receptors. Second-generation antihistaminics are lack of sedating activity due to their weak brain penetration.
Certain H1 antihistamines are effective in preventing motion sickness. It’s unclear whether this is due to histamine antagonism in the brain or because these compounds have antimuscarinic properties.
Promethazine and few other antihistamines reduce tremor, rigidity and sialorrhea of parkinsonism.
Some older antihistamines, particularly cyproheptadine, have a stimulant effect on appetite.
PHARMACOKINETICS
H1 antihistamines are well absorbed by oral and parenteral routes, metabolized in the liver, and eliminated in the urine. Duration of action of most agents is 4–6 hours, except meclizine, chlorpheniramine, Mizolastine, loratadine, cetirizine and fexofenadine which act for 12–24 hours or more.
SIDE EFFECTS AND TOXICITY
Side effects of first generation H1 antihistaminics are frequent, but usually mild.
CNS depressive effects such as sedation, decreased attention and focus, light headedness, motor incoordination, fatigue, and a tendency to fall asleep are the most common. Patients should be advised not to drive or use machinery that requires constant attention. Individuals differ significantly in their susceptibility to drug side effects. With frequent use, some tolerance to side effects develops. CNS effects are virtually absent in second-generation drugs. Regular use of conventional antihistamines is not recommended in children since it may interfere with learning and academic tasks.
Anticholinergic side effects include dry mouth, urinary hesitancy, bowel movement alterations and blurring of vision. these are common with promethazine, pheniramine, diphenhydramine, and dimenhydrinate. Acute overdose produces central excitation, tremors, hallucinations, muscular incoordination, convulsions, flushing, hypotension, fever and some other features of belladonna poisoning.
Second generation antihistaminics
Second-generation antihistaminics are H1 receptor blockers that were launched after 1980 and have one or more of the following characteristics:
• There is no CNS depressive effect. These newer drugs have the advantages of not impairing psychomotor performance, causing no lethargy, and not potentiating effect of alcohol or benzodiazepines.
• Lack of anticholinergic side effects, as higher H1 selectivity.
• In addition to histamine blockage, several drugs also decrease late-phase allergic reactions by acting on leukotrienes or by inhibiting platelet activating factor.
H1 ANTIHISTAMINES USES
1. Allergic rhinitis and conjunctivitis, hay fever, pollinosis. They control sneezing, runny but not blocked nose, and red, watering, itchy eyes.
2. symptomatic relief in insect bite and ivy poisoning.
3. Urticaria, dermographism, atopic eczema.
4. Acute allergic reactions to drugs and foods.
5. Pruritis – Many antihistamines have antipruritic properties independent of H1 antagonistic activity. Though relief is often incomplete, older antihistamines chlorpheniramine, diphenhydramine, cyproheptadine are still the first-line drugs for idiopathic pruritus.
6. Common cold and cough– Antihistaminics do not affect the course of the illness but may provide symptomatic relief (reduce rhinorrhoea) by anticholinergic and sedative actions. Many cough medicines contain antihistamines such as chlorpheniramine, diphenhydramine, and promethazine.
7. Motion sickness –Promethazine, diphenhydramine, dimenhydrinate and meclizine have prophylactic efficacy in milder types of motion sickness and advised to take one hour prior to journey.
8.Vertigo – Cinnarizine is an antihistamine with additional anticholinergic, anti-5-HT, sedative, and vasodilator effects that is commonly used to treat vertigo. It regulates Ca2+ fluxes and inhibits the vasoconstrictor effects of a variety of endogenous mediators.
9. Acute muscular dystonia – Parenteral promethazine, diphenhydramine, or hydroxyzine relieves acute muscular dystonia produced by antidopaminergic-antipsychotic medications. This is due to the drugs’ central anticholinergic activity.