Histamine, which means ’tissue amine’ (histos—tissue), an autacoid, found in universally all animal tissues. Histamine is mostly found in mast cell storage granules. Histamine produced by non-mast cells can be found in the brain, gastric mucosa, epidermis, and growing regions. Mast cell histamine turnover is sluggish, whereas non-mast cell histamine turnover is rapid. Blood, most bodily secretions, venoms, and pathological fluids all contain histamine. Histamine is a mediator of inflammation-induced vasodilation and other responses. Histamine serves a key role to mediate hypersensitive reactions.
histamine Storage and destruction
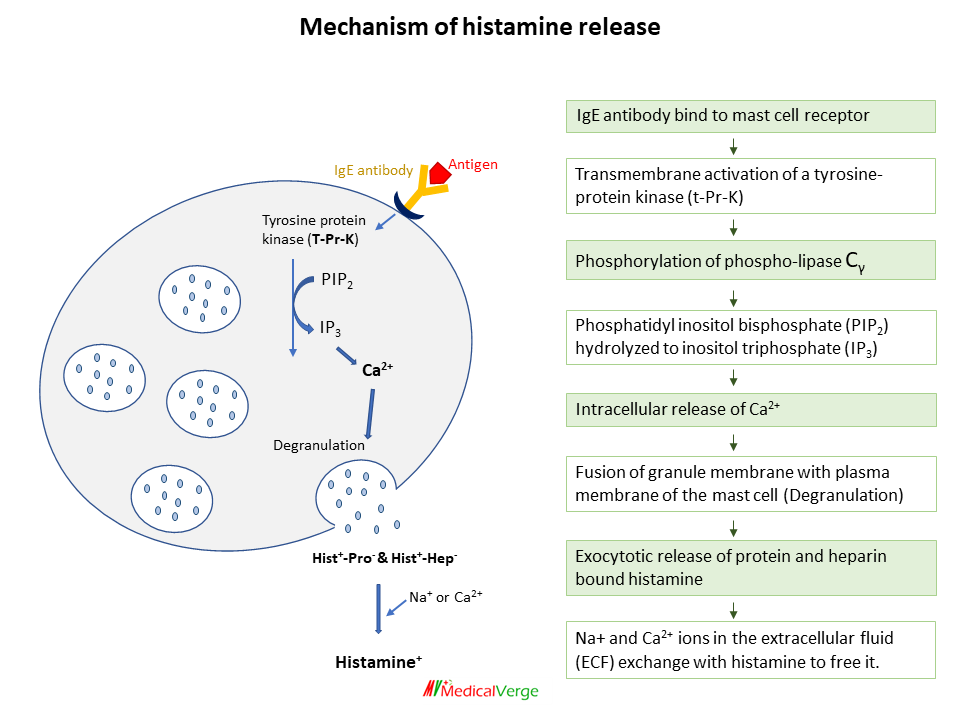
Histamine (a positively charged molecule) is retained within intracellular granules by an acidic protein and heparin (a negatively charged molecule) in mast cells. When granules are released via exocytosis, Na+ ions in the extracellular fluid (ECF) exchange with histamine to free it.
Histamine release is inhibited by an increase in intracellular cAMP (driven by adrenergic agonists and methylxanthines). Orally, histamine is inactive because histamine absorbed from the intestines is degraded by the liver.
Histamine receptors
Four different types of histaminergic receptors have been identified and cloned. These are H1, H2, H3 and H4. H1 antagonists are used to treat allergies, while H2 blockers are used to treat acid reflux and peptic ulcer disease. Although it has no clinical utility, the H3 receptor functions largely as a presynaptic autoreceptor, controlling histamine release from neurons in the brain. The chemotaxis of Eosinophils, mast cells, and basophils is enhanced when H4 receptors are activated. The H4 receptor may have a role in allergic inflammation, and H4 antagonists are being investigated as potential treatments for allergic inflammatory diseases such as rhinitis and asthma. Though the H4 receptor is pharmacologically less distinct with H2 agonist.
PHARMACOLOGICAL ACTIONS
Blood vessels
Histamine induces a significant dilation of smaller blood vessels such as arterioles, capillaries, and venules (partly by direct action through the H2 receptor and partly by indirect action through the H1 receptor mediated ‘endothelium dependent relaxing factor’ (EDRF)/NO).Histamine increases capillary permeability by separating endothelial cells, resulting in plasma exudation (primarily H1 response). While Histamine constricts larger arteries and veins (mediated by H1 receptor on vascular smooth muscle).
Visceral smooth muscle
Histamine promotes bronchoconstriction as smooth muscle contraction by H1 response.
Glands
Through direct action on parietal cells via H2 receptors, histamine induces a significant increase in gastric acid secretion.
CNS
Histamine does not penetrate blood brain barrier (BBB). Intracerebroventricular administration, on the other hand, causes behavioural arousal, vomiting, hypothermia, a rise in blood pressure, cardiac stimulation, and ADH release in animals. Both H1 and H2 receptors are responsible for these actions.
In the brain, histamine is thought to be the afferent transmitter, notably in the hypothalamus and midbrain. It aids in the maintenance of wakefulness and the suppression of appetite. H1 antihistaminics are known for their sedative and appetite-stimulating properties.
Tissue growth and repair
Because growing and regenerating tissues contain high amounts of histamine, it has been postulated that it plays an important role in the process of growth and repair.
Sensory nerve endings
Histamine stimulate nerve endings, which causes itching and pain.
Allergic phenomena
Histamine produced by mast cells has a critical function in IgE-mediated hypersensitivity reactions. The triple response elicited by the H1 response is: 1) Red patch (due to severe capillary dilation), 2) Wheal (due to fluid exudation from capillaries and venules), and 3) Flare (redness in the surrounding area) due to arteriolar dilatation mediated by axon reflex.
Histamine USES
Histamine has no medicinal value. Betahistine is an orally active H1 selective histamine analogue used to treat vertigo in Meniere’s disease. Betahistine is thought to work by inducing vasodilation in the inner ear. It’s not recommended for asthmatics or people who have ulcers. In contrast, anti-histaminic medications are used for a variety of purposes.
HISTAMINE RELEASERS
Mast cells can release histamine in response to a number of mechanical, chemical, and immunological stimuli –
1) Tissue damage like trauma, stings or venoms, proteolytic enzymes.
2) Antigen-antibody reaction due to IgE antibodies.
3) Polymers like dextran, polyvinyl pyrrolidone (PVP).
4) Surface acting agents such as compound 48/80, Tween 80.
5) Basic drugs such as atropine, morphine, vancomycin, tubocurarine, polymyxin B, pentamidine and even some antihistaminics directly release histamine without triggering an immune response.