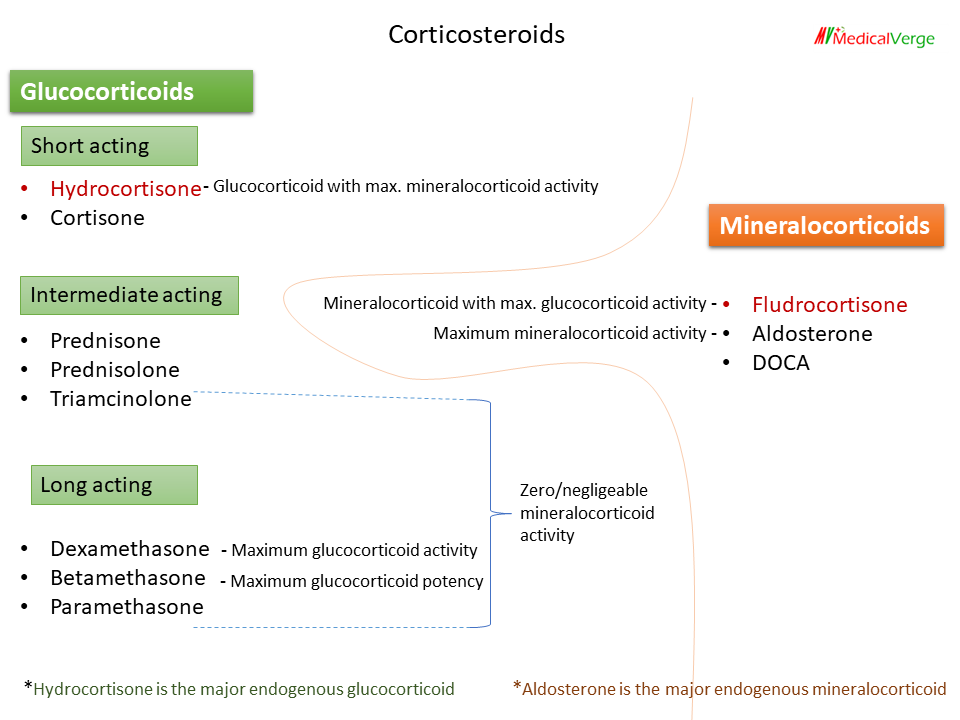
Steroids or Corticosteroids are hormones produced by the adrenal cortex and are necessary for various physiological functions in the body. The terms ‘corticosteroid’ and ‘corticoid‘ are used interchangeably to refer to natural gluco- and mineralo-corticoids, and their synthetic analogues. Hydrocortisone is the major endogenous glucocorticoid, whereas aldosterone is the major endogenous mineralocorticoid. The key role of glucocorticoid is to maintain glucose supply to the brain and anti-inflammatory activity. Mineralocorticoid is responsible for maintaining electrolyte balance.
Action of corticosteroids
Corticosteroids have both direct and permissive actions. By permissive action is meant that they do not themselves produce an effect but their presence facilitates other hormones to exert that action. For example, they have no direct effect on blood pressure, but their absence markedly blunts the pressor activity of adrenaline.
Mineralocorticoid action
Retention of Na+ and H2O, while excretion of K+ and H+ as in exchange with sodium through DCT in nephrons. Conditions associated with hyperaldosteronism such as in Cushing syndrome and Conn’s syndrome, there is hypokalemia and alkalosis. While hypoaldosteronism like Addison’s disease manifests as hyperkalemia and metabolic acidosis.
Glucocorticoid action
1. Catabolic action
Glucocorticoid Promote glycogenesis and gluconeogenesis in the liver, while inhibit glucose utilization by peripheral tissues. This causes hyperglycemia and insulin resistance, which mimics diabetes. So avoided in diabetes mallitus.
Breakdown of protein, which used up in gluconeogenesis, causes excess urea production and negative nitrogen balance. Glucocorticoid excess can manifests as myopathies.
Glucocorticoids have a permissive effect on fat metabolism. They promote lipolysis due to glucagon, growth hormone, Adrenaline and thyroxine. Different area of the body responds differently, causing redistribution of fat. In a condition of glucocorticoid excess, there is fat breakdown at peripheral area and deposition in the face, neck, and shoulder, resulting in ‘moon face’, ‘fish mouth’, and ‘buffalo hump’.
Glucocorticoids inhibit intestinal absorption and enhance renal excretion of Ca2+, causes indirect loss of calcium from bone, may result in osteoporosis.
2. Anti-inflammatory action
Glucocorticoid suppress almost all stages of inflammation, irrespective of the type of injury. Chemotaxis inhibition is the primary mechanism of anti-inflammatory action. They have the potential to cause delayed wound healing.
3. Effect on blood
All blood cells are produced in the bone marrow and then transported to the bloodstream. Glucocorticoids promote neutrophil transport from bone marrow to blood, resulting in neutrophilia, whereas they inhibit lymphocyte movement from bone marrow to blood, resulting in lymphopenia.
Uses of glucocorticoid
Corticosteroids are given by a various routes, including inhalation, topical, intranasal, and systemically (oral and parenteral), depending on the condition to achieve higher concentration at the site of action.
1. Antenatal use
Dexamethasone or betamethasone is provided for foetal lung maturity because glucocorticoids stimulate surfactant production.
Betamethasone – 12 mg, i.m. 2 doses 24 hour apart.
Dexamethasone – 6 mg, i.m. 4 doses 12 hour apart.
2. Replacement uses
Acute adrenal insufficiency – It is an emergency condition. Hydrocortisone or dexamethasone are given i.v., first as a bolus injection and then as infusion.
Chronic adrenal insufficiency (Addison’s disease) – Oral hydrocortisone is the most frequently prescribed medication.
3. Diagnostic use
The dexamethasone suppression test is used to determine whether high levels of steroid in the blood are related to Cushing syndrome or a natural physiological process. The dose of 1 mg dexamethasone is given at 11 p.m., and the cortisol level is evaluated the next morning (8 AM). A cortisol level of less than 3 indicates normal physiological rise (suppression occurred), whereas a level of more than 5 indicates Cushing syndrome.
4. Other uses
- As an anti-inflammatory agent in a wide range of inflammatory disorders, including arthritis, gout, and rheumatic carditis.
- As an immune-suppressant in transplantation and various autoimmune diseases.
- Anti-cancer treatment, such as for Hodgkin lymphoma (HL), Multiple Myeloma (MM), NHL, LL etc.
- Bronchial asthma.
- The cough associated with postnasal drip of sinusitis

Measures to avoid HPA axis suppression
When corticosteroids are given continuously for more than two weeks, the HPA axis is suppressed. Symptoms of “steroid withdrawal syndrome” include lassitude, musculoskeletal pains, and, occasionally, fever. The following actions must be taken:-
• Stop unnecessary use of steroids.
• If necessary, prescribe them for a period of less than two weeks.
• If they’re needed for a long period, give them on alternate days. Long-acting steroids should be avoided.
• If daily and longer periods are indicated, don’t stop abruptly; tapering should be done.
If a person has been taking steroid for several months and develops an infection or requires emergency surgery, the steroid should not be stopped. Because the person is suffering from HPA suppression, which is a life-threatening condition, and the infection is treatable with antibiotics.