Drugs derived from opium (poppy plants) are called opiates e.g., morphine, while opiates like substances are called opioids. Opioids are semi-synthetic or synthetic substances having similar characteristics and the ability to interact with opioid receptors in the brain. There are 3 receptors µ (mu), κ (kappa) and δ (delta) for opioids. All three receptors (µ, κ, δ) have analgesic action. µ-receptors are responsible for euphoria while κ-receptors are responsible for causing dysphoria. Stimulation of δ-receptors shows affective behavior and reinforcing action.
Opioids, which include drugs like morphine, fentanyl, and tramadol, are commonly used to relieve pain. They are centrally acting analgesics that are useful in cases where NSAIDs are ineffective, such as visceral pain. It inhibits the release of excitatory transmitters (such as substance P) from primary afferents carrying pain impulses in the substantia gelatinosa of the dorsal horn. Miosis is developed when the Edinger Westphal nucleus of the III nerve is stimulated. No miosis occurs on topical application of morphine to the eye.
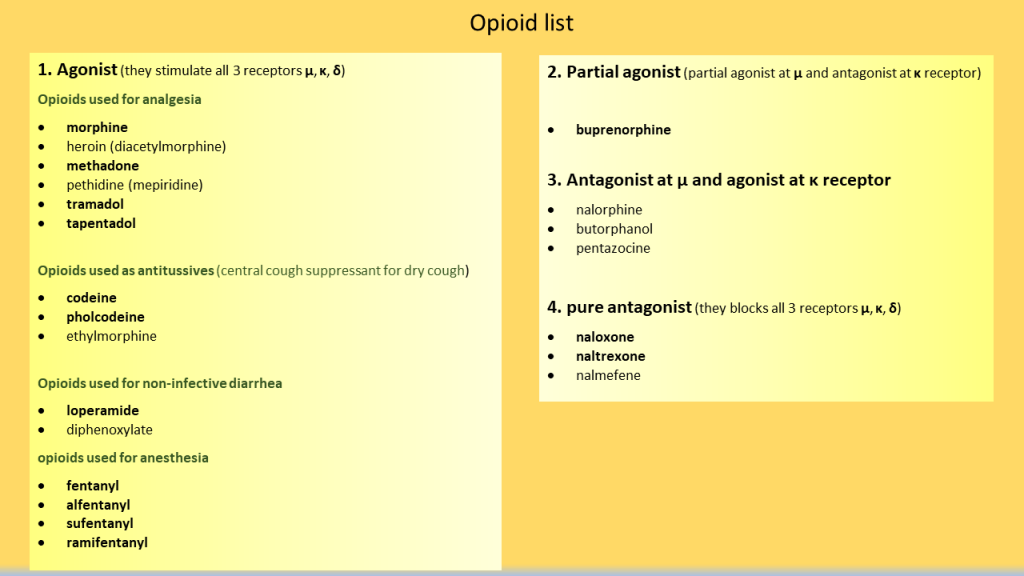
opioid classification
1. Agonist (they stimulate all 3 receptors mu, kappa and delta)
Opioids used for analgesia
- morphine
- heroin (diacetylmorphine) – 100 times more addictive than morphine, so not used clinically.
- methadone – very long acting, so used for deaddiction of opioid dependence.
- pethidine (mepiridine)
- tramadol
- tapentadol
Opioids used as antitussives (central cough suppressant for dry cough)
- codeine
- pholcodeine
- ethylmorphine
Opioids used for non-infectious diarrhea
- loperamide
- diphenoxylate
Opioids used for anesthesia
- fentanyl
- alfentanyl
- sufentanyl
- ramifentanyl
2. Partial agonist (partial agonist at mu and antagonist at kappa receptor)
- buprenorphine
3. Antagonist at mu and agonist at kappa receptor
- nalorphine
- butorphanol
- pentazocine
4. Pure antagonist (they blocks all 3 receptors mu, kappa and delta)
- naloxone
- naltrexone
- nalmefene
Opioid dependence
Opioid dependence can develop as a result of non-medical use, chronic use, misuse, and use without medical supervision. Opioid replacement, such as with methadone and buprenorphine, is used for maintenance of opioid addiction. The most usual method is to reduce opioid doses followed by symptomatic treatment for withdrawal symptoms such as joint pain, rhinorrhea, and constipation.
Opioid overdose
Naloxone can prevent mortality from an opioid overdose, If given in time. A combination of three signs and symptoms can indicate an opioid overdose: pinpoint pupils, unconsciousness, and breathing difficulties.
Tolerance
If morphine and related opioids are used frequently, a high degree of tolerance can develop. It’s partly pharmacokinetic (rapid metabolism), but mostly pharmacodynamic (cellular tolerance).Tolerance is exhibited to most actions, but not to constipating and miotic actions.
Actions
Miosis is developed when the Edinger Westphal nucleus of the III nerve is stimulated. No miosis occurs on topical application of morphine to the eye.
Opioid receptors are abundant in the enteric plexus neurones and gastrointestinal mucosa. Direct action on the intestines and in the CNS raises tone and segmentation while lowering propulsive movements. It is possible to elevate the tone of the duodenum and colon to the level of spasm. There may be spasm of pyloric, ileocaecal and anal sphincters. Decrease in all gastrointestinal secretions due to reduction in movement of water and electrolytes from mucosa to the lumen, result in constipation.
Morphine depresses respiratory centre in a dose dependent manner.
Nausea and vomiting occur as side effects. Morphine appears to sensitize the CTZ. However, larger dosages directly depress the vomiting centre, therefore emetics should not be used in morphine intoxication.
Morphine causes vasodilatation due to histamine release and depression of vasomotor centre. There is a shift of blood from pulmonary to systemic circuit due to greater vasodilatation in the latter. The decrease in peripheral resistance reduces cardiac effort, giving morphine an anti-ischemic effect.